T-cell antigen receptors are only present on the cell membrane. We will learn more about T Cell Receptors (TCRs) in this blog.
T cells or T lymphocytes have protein complexes called TCRs that are found on their surface and are in charge of identifying antigens on foreign substances. Without TCRs, the immune system would be unable to identify and combat infectious diseases.
We will discuss about the Pluribead cascade straining and how it helps in the separation of TCRs.
Structure of TCRs
T cell receptors are members of the immunoglobulin family, which is a large group of proteins that bind to and recognize antibodies. TCR chains contain complementarity-determining regions (CDRs), which determine which antigens the TCR will bind to.
TCRs typically have an alpha and a beta chain. They develop in the thymus, where their DNA is recombined to form new TCRs. If the process is successful, the cells’ alpha-chain DNA will be rearranged to produce functional alpha-beta TCRs. T cells with functional and stable TCRs and CD8+ receptors can undergo positive or negative selection:
- Positive selection enables T cells to bind to foreign antigens.
- Negative selection – T cells may bind too strongly, resulting in autoimmunity.
- T cells of various types can have gamma and delta receptor chains. This is a less common combination that results in CD3+ cells that activate CD4+ and CD8+ cells. There is also a variation in the markers of self-antigens vs. non-self antigens.
Function of TCRs
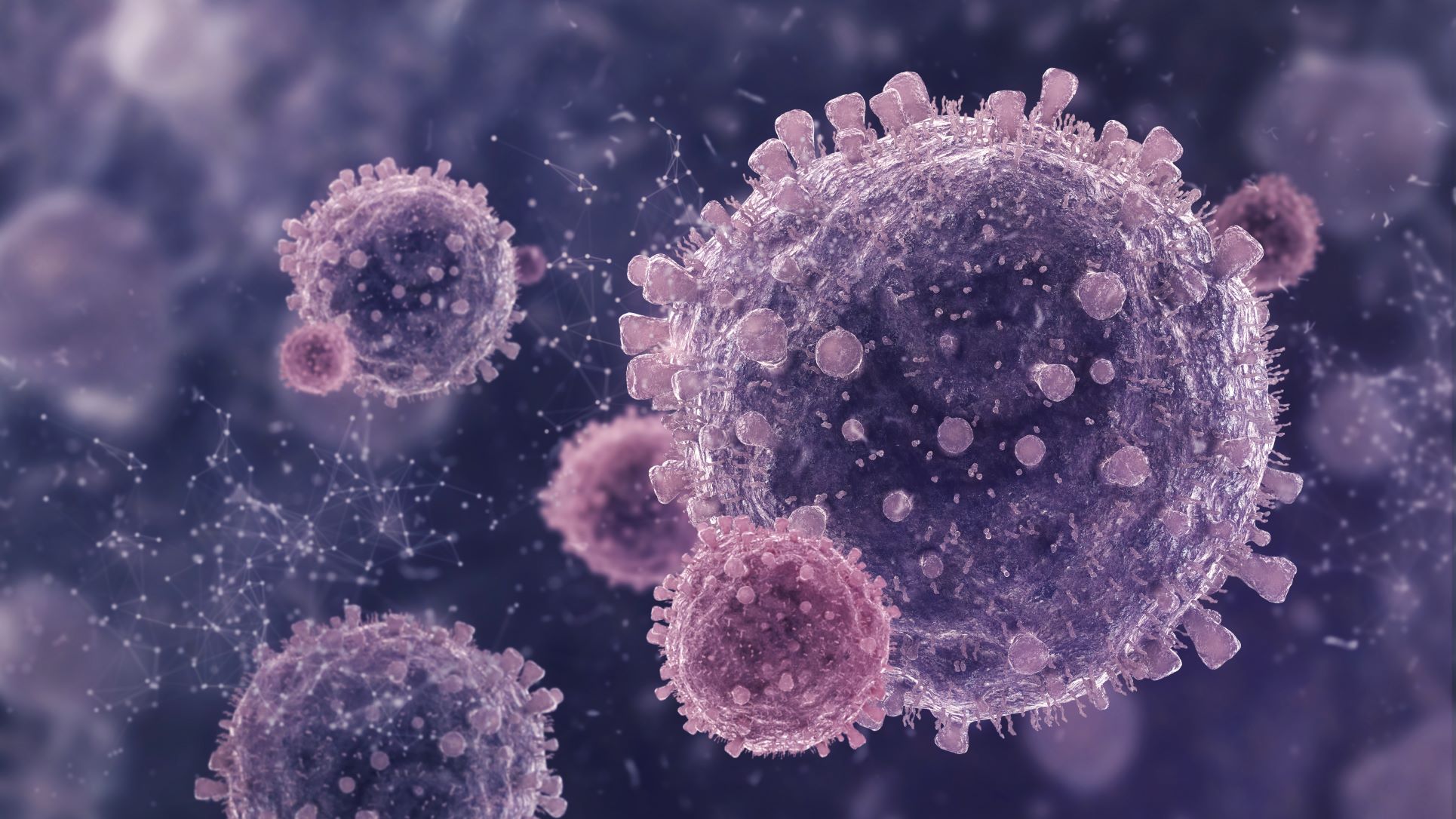
When a virus successfully attaches to a cell, the T cell’s defense system activates to kill the infected cell. The substance must first enter the body by infecting it. Once inside the bloodstream, the virus can attach to the cells and take root.
T Cell receptors can bind to foreign protein fragments attached to the surface of body cells. This allows them to develop into a variety of cells that are essential in the immune response. Carefully attacking virus-infected cells while avoiding healthy cells.
Cytotoxic T cells and helper T cells are two types of mature T cells that are involved in the processes:
- Cytotoxic T cells kill cells that are harmful to the body, such as cancer cells, viruses, and bacteria.
- Helper T cells activate other cells and direct them to the appropriate site.
The life cycle of T cells
T cells
When T-cell precursors leave the bone marrow to mature in the thymus, they lack antigen receptors and are thus insensitive to antigen stimulation. T cells multiply many times within the thymus as they pass through a meshwork of thymus cells. They acquire antigen receptors and differentiate into a helper or cytotoxic T cells as they multiply. These cell separation can be done as per their function and the presence of special surface proteins called CD4 and CD8. Most T cells that multiply in the thymus die there as well. This may seem wasteful until one realizes that a significant portion of the antigen receptors produced at random are self-antigen receptors, which are molecules present in the body’s own components, and that mature lymphocytes equipped with these receptors would attack the body’s own tissues.
Because most self-reactive T cells die before leaving the thymus, the T cells that do emerge are capable of recognizing foreign antigens. These travel through the blood to lymphoid tissues, where they can multiply and participate in immune responses if properly stimulated. T cell production in the thymus is an ongoing process in young animals. Humans produce a large number of T cells before birth, but production gradually slows down during adulthood and is greatly reduced in old age, by which time the thymus has shrunk and partially atrophied. Cell-mediated immunity, on the other hand, lasts throughout life because some T cells that emerge from the thymus continue to divide and function for an extended period of time.
Activation of TCRs
When T cells bind to MHC molecules, they produce functional TCRs. This requires the CD4 or CD8 co-receptors to signal the reaction to bind. T cells that can bind to a peptide chain in the thymus are released into the peripheral lymphoid organs. If the naive T cells do not come into contact with the activation antigens, they will be unable to multiply, rendering them ineffective.
Pluribead For T Cells Separation
This research can be simplified by streamlining various stages of the manufacturing process. T-cell separation takes a long time and requires expensive equipment.
Previously, researchers used complex machines to perform the time-consuming task of sorting and purifying large volumes of T cells. Innovative cell separation strategies, such as Pluribeads, are more efficient and produce better results at a lower cost.
Pluribead cascade straining tool operates without the use of any magnetic components, aids in the gentle and safe isolation of T Cells. The procedure is straightforward: your pluriBeads (which contain bound target cells) are sieved through a strainer, with unwanted cells passing through and your target cells remaining on top. After detaching, you are now ready to proceed with your target cells.
Two Different Bead Sizes are Available
- S-pluriBead: It is applied to a limited number of targets in large sample volumes.
- M-pluriBead: A material that is versatile and can be used to achieve multiple goals while using less material.
Our team of scientific experts is committed to the success of the researchers with whom we collaborate. We look forward to providing you with our novel pluriBeads technology so that you have the best tool for your next great scientific breakthrough.
Reference
Nature
Britannica
 English
English French
French
 German
German
 Spanish
Spanish
 Belgium
Belgium
 Italian
Italian Brazil
Brazil Chinese Mandarin
Chinese Mandarin